Imagine a world where recovery from addiction isn’t just possible but is guided by groundbreaking counseling techniques that are revolutionizing the field. That’s right, addiction recovery is undergoing a radical transformation, making it more effective than ever.
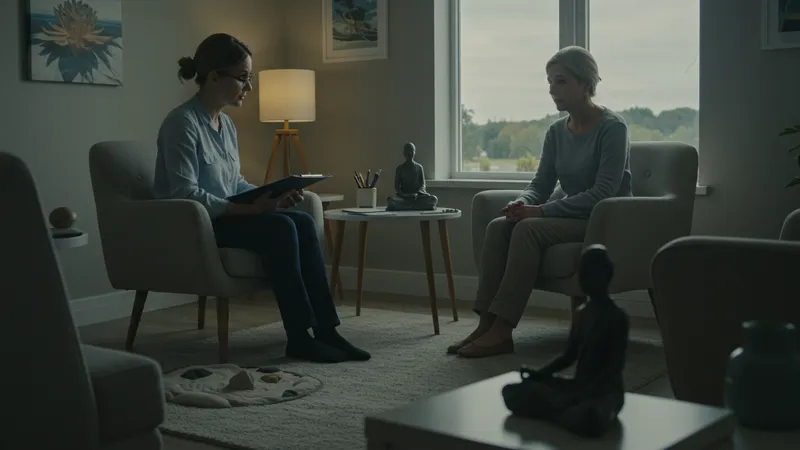
In today’s fast-paced and often isolating society, substance abuse has reached alarming levels. But here’s the twist: integrated health services are proving to be the unexpected game-changer, combining counseling with holistic therapies to tackle addiction from every angle.

Surprisingly, the combination of traditional therapy methods with integrated health services isn't just a trend—it's cementing itself as the future of addiction recovery. By addressing the root causes of addiction with a multi-disciplinary approach, these programs are achieving success rates previously thought impossible. Imagine pairing counseling with yoga and nutritional advice, all scientifically backed to enhance well-being and support long-term recovery. But that’s not even the wildest part…
What sets these programs apart is their focus not only on detoxification but on empowering individuals to rebuild their lives entirely. Picture receiving personal coaching to develop life skills alongside your recovery journey, something previously neglected in addiction treatment. This paradigm doesn’t just treat symptoms; it transforms lives. Ready for the most jaw-dropping revelations? What happens next shocked even the experts…
In the new age of addiction recovery, counseling plays a more vital role than ever. But did you know that even the traditional approach has undergone a complete makeover? Modern therapy now integrates cognitive behavioral therapy with mindfulness practices, creating a hybrid technique that's yielding unprecedented results. Mindfulness helps patients stay rooted in the present, reducing the cravings and triggers that derail progress.
These enhanced counseling strategies aren't just invigorating recovery; they're also proving to be cost-effective. Facilities offering these services have seen a marked reduction in relapse rates—a major saving on the societal costs of unresolved addiction. But there’s one more twist to how these approaches are reshaping perception and treatment of addiction...
Imagine a treatment center where diverse practitioners work together under one roof: psychologists, nutritionists, yoga instructors—all part of a single, unified treatment plan. This isn’t just theoretical; integrated centers are popping up worldwide, fostering a collaborative environment where comprehensive care is not just a goal but a reality. This symbiotic care approach is the next frontier, pushing beyond individual therapies to create a holistic recovery ecosystem.
What you read next might change how you see this forever. While this multi-faceted support is overwhelming positive, it raises questions about the accessibility and affordability of such comprehensive care. How can these groundbreaking treatments become universally available? Prepare yourself for an exploration of these solutions in the upcoming pages.
Despite the promising potential of integrated health services in addiction recovery, accessibility remains a challenge. Many people face barriers such as financial limitations, geographic locations, and social stigma. These hurdles can often deter individuals from seeking the help they desperately need. But there are innovative strategies emerging to dismantle these barriers, one step at a time.
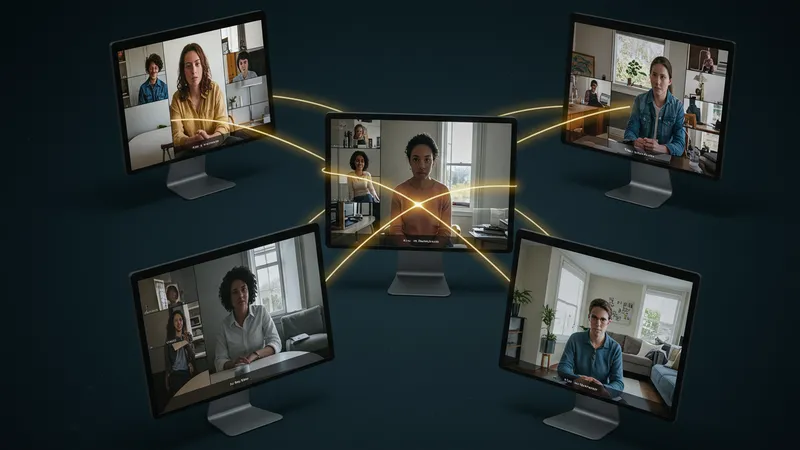
Telehealth services have become a beacon of hope for many. Offering remote access to therapy, they bridge the gap for individuals in rural areas where in-person treatment options are scarce. But there's more: state-funded programs are increasingly incorporating telehealth options, making mental health services more accessible than ever before. But that’s not all there is to the story...
Financial constraints are another significant barrier that must be addressed. To combat this, more centers are adopting a sliding scale payment model, ensuring that no one is turned away due to cost. Additionally, governmental initiatives are underway to increase funding for mental health services, aiming to ensure that the high-quality integrated care approaches become a standard, not a luxury.
Hang onto your seat, because what comes next may revolutionize how we think about addiction recovery and societal support. As the demand for integrated services grows, communities are rallying to create local support networks that extend beyond professional help. These networks are forming a new safety net, one that enables sustainable recovery by fostering community involvement.
The community is often an overlooked asset in the recovery process, yet its role is undeniably powerful. Support groups and local initiatives can make a monumental difference, transforming how individuals perceive and engage with their addiction. Newsflash: Community-driven recovery groups are gaining traction, providing an invaluable support structure outside traditional healthcare settings.

These groups often utilize peer-led models that promote shared experiences as a backdrop for healing. Surprisingly, stats show that community-based programs can double the success rate of recovery efforts, creating lasting behavioral change. Engaging in collective activities, such as group outings or volunteer works, helps in building a sense of belonging and purpose, both critical for a successful recovery process.
One might wonder why more facilities aren't embracing this community-first model. The reality? Shifting traditional institutions to include community-oriented approaches requires a fundamental change in mindset and practice. Despite the challenge, there's a growing acknowledgment of the immense benefits pilot programs have shown, urging more facilities to consider this path.
But the real eye-opener is still to come. The integration of community support with professional treatment is not just enhancing recovery outcomes but is also creating a ripple effect, improving overall community well-being. Curious about what happens when entire neighborhoods rally to support their residents? The next page tackles that very question.
When communities step up to support addiction recovery, the benefits flow in both directions. Holistic recovery initiatives do more than just help individuals—they rejuvenate entire communities. It's an unexpected cycle of positive influence and reciprocal growth. The ripple effects of successful recovery initiatives can be observed in decreased crime rates and enhanced social cohesion, making communities safer and more cohesive.

Consider this: communities involved in supporting addiction recovery often experience a boost in their own mental health and resilience. As individuals overcome addiction, they often become advocates, sharing their wisdom and experiences, which, in turn, strengthens community bonds. These individuals might even contribute economically through employment and volunteering, turning their recovery into a community asset.
The societal stigma surrounding addiction has long been a barrier to recovery, but communities are gradually transforming this narrative. With awareness programs and education campaigns, social norms are shifting toward understanding and compassion rather than judgment. Local laws are evolving too, with community-inspired policies aimed at fostering supportive environments for recovery.
But the most astonishing facet to emerge is how these changes are laying the foundation for future generations. Communities that have seen successful addiction recovery initiatives are incorporating lessons learned into educational programs and youth outreach, aiming to prevent substance abuse before it starts. What could this mean for the future of addiction recovery? Let's peel back another layer in the next segment.
Preventing addiction before it even begins is a concept that takes addiction recovery to an entirely new level. Integrated health services, traditionally seen as tools for recovery, are now being harnessed as means of prevention, particularly among the youth. But how effective can these services be in stopping addiction in its tracks before it even begins?
By focusing on mental health education and resilience-building strategies within schools, these services provide young individuals with tools to make informed choices. Programs now feature comprehensive education on the impact of substance abuse and emphasize emotional and mental wellness. The surprising part? There's evidence to suggest that early intervention can cut future addiction rates by half.
But why stop at schools? Community programs are equally essential in this early intervention stage. Family counseling services offered through integrated health centers give parents the tools they need to support their children effectively. These interventions not only educate but empower families to become proactive contributors to both individual and community health.
What could potentially revolutionize youth prevention even more? The integration of cutting-edge technology into these programs. Virtual reality therapy is emerging on the scene, teaching emotional coping mechanisms in an immersive environment. Is the future of addiction prevention here? The next section might just rewrite everything you know.
Virtual reality (VR) is not just for gamers—it’s transforming the landscape of addiction recovery. Prepare to have your preconceptions challenged, as VR creates immersive experiences that allow individuals to confront triggers and develop healthier responses in a safe, controlled environment.

Using VR in therapeutic settings offers a unique opportunity to simulate real-world challenges. Patients can safely experience scenarios that might trigger cravings and rehearse coping strategies, making them better prepared when they encounter similar situations in real life. It’s a form of habituation therapy that’s groundbreaking in its application, and studies show VR therapy can boost recovery rates significantly.
Moreover, the allure of VR isn't limited to its effectiveness; it's also incredibly engaging. Eliciting cooperation from patients who might otherwise be hesitant to participate in traditional therapy becomes feasible when the method involves technology they are eager to explore. Therapists report increased patient engagement and improved therapy retention with VR.
But the most fascinating part of this tech integration is how it might democratize access to therapy. With proper funding and technological advancement, VR-assisted therapy could become more widely available, lowering costs and broadening access. What's the secret technology driving this transformation, you ask? More on that pioneering innovation in the next segment.
Artificial Intelligence (AI) and machine learning promise to leap beyond conventional therapeutic boundaries in addiction recovery. These technologies offer personalized treatments, adapting to an individual's progress and needs dynamically—something traditional methods could only dream of.
By analyzing vast amounts of data, AI systems can identify patterns and predict relapse triggers more accurately than ever before. The algorithms become powerful allies in the hands of therapists, offering insights that wouldn't be evident through human observation alone. With AI's help, treatment plans can become not only tailored but also predictive, offering pre-emptive interventions.
Integrating machine learning into therapy has shown promising improvements in diagnosing co-occurring disorders, often unnoticed in initial assessments. This adds a new dimension to personalized care, wherein dual-diagnosis is nuanced, offering precisely tailored therapies for each layer of complexity in mental health.
However, the implications stretch far beyond therapeutic precision. The technology is set to transform administrative operations, making it possible for centers to operate more efficiently and affordably. Imagine a future where AI streamlines operations to such an extent that high-quality care becomes universally accessible. What’s the potential impact on treatment costs? Brace yourself for what lies ahead.
One of the biggest challenges in addiction recovery has always been cost. Now, technological innovations are driving down expenses, making comprehensive treatment programs more accessible to more people. This affordability revolution is not just about cutting corners—it's about optimizing resources.

Automating administrative tasks through AI significantly reduces overhead costs, allowing treatment centers to allocate more resources to direct patient care. This not only leads to more focused, patient-centered services but also enables centers to function with greater efficiency and less waste.
Moreover, telehealth options are increasingly being integrated into recovery programs, reducing the need for costly in-person sessions. These digital consultations have proven to be not only more affordable but, in many cases, equally effective as face-to-face therapies. But there's still one more fascinating development on the horizon that could change everything...
What if the key to universally affordable care wasn't just about cost reduction but about increasing personal investment in recovery itself? More facilities are exploring crowd-funded healthcare models, where communities pool resources to ensure members have access to the care they need. In this way, care becomes both a personal and collective responsibility. What this could mean for global health initiatives is profound, and we're just beginning to scratch the surface.
When it comes to financing addiction treatment, a shift in strategy can shake the foundations of what's financially possible. What if individuals and communities took the reins of funding? Enter social finance models and crowd-funded healthcare as groundbreaking paradigms.

These approaches are allowing treatment centers to operate with not just community backing but active community involvement, fostering a sense of collective ownership over health outcomes. Crowdfunding not only democratizes access to care but connects donors directly to positive societal change, creating a virtuous cycle of support and healing.
Some centers are also exploring partnerships with tech innovators, banks, and philanthropists to create fund-matching models where every dollar raised is doubled by corporate philanthropy. Imagine the potential impact: shared financial responsibility that could sustain and expand treatment opportunities globally—a model of endless possibility.
Yet, while revolutionary, these approaches must contend with traditional funding mechanisms. The intersection of innovation with public and private funding is a complex dance, requiring new policies and thoughtful regulation to flourish. Could these reborn financial models pave the way for universally accessible recovery services? Up next: a closer look into global implications and what's needed to make visionary funding a reality.
Envision a world where scalable integrated recovery services are available to anyone, anywhere. It’s a lofty dream, but not unachievable, thanks to the frameworks being set up today. As technological advances blend seamlessly with creative funding solutions, the untapped potential of global treatment networks becomes apparent.

The momentum for scalable solutions is gaining traction with international collaborations between health organizations, tech firms, and governments. By sharing resources and best practices, these global partnerships aim to create adaptable models of care that respect cultural nuances while maintaining effective standards.
Education and technology exchange programs are key facets in this international strategy. Countries with advanced healthcare systems can assist by sharing both tech and expertise with under-resourced nations, enabling them to fast-track the development of integrated services that meet local needs.
Yet, for these grand visions to become reality, strategic alignment among stakeholders is essential. Regulation, ethical considerations, and open dialogue must guide the evolution of global recovery services. What lies beyond current challenges? Eye-opening lessons from another industry reveal just the alchemy needed for crossover healing success.
The fitness industry may seem an odd place to look for breakthroughs in addiction recovery, but parallels between physical and mental health reveal untapped synergy. Personalized, tech-driven solutions pioneered by fitness apps can inform new addiction care approaches. Could motion tracking in VR be the next evolution in therapy engagement?

Indeed, the emphasis on personal empowerment that fitness technologies foster can translate into mental health wins, too. With apps reminding users of exercise and meditation routines, maintaining mental health hygiene becomes habitual, promoting a holistic approach toward self-care.
Gamification—a tool frequently used within fitness apps—also has potential applications. Reward-based systems keep individuals engaged, turning therapy into an interactive experience rather than a stringent chore. Progress tracking, badges, or social sharing can offer motivation and community, echoing the successful strategies in physical health.
The true breakthrough from fitness might be its flexible model: accessible, on-demand services with community at their core. These elements mirror exactly what expanded mental health services require. What happens when addiction recovery adopts such agility? Join me as we speculate what's next.
With technology, community involvement, and personalized care converging, the stage is set for an innovation wave unlike any seen before in addiction recovery. What radical invention might be just over the horizon to further redefine care strategies worldwide?
The potential of Artificial General Intelligence (AGI) looms large—a tool capable of understanding individual needs beyond current constraints, with the capacity to orchestrate seamless, intuitive therapy plans across multiple platforms. Such intelligence could hyper-personalize self-care in real-time, tracking progress with unrivaled precision.
Explorations into biofeedback technology are gathering steam, too. Integrating real-time biometric data into therapy sessions could prepare therapists for proactive interventions, augmenting traditional talk therapy with physiological insights for holistic healing.
The real groundbreaker, though, might lie in the ethical openness of technological integration. Navigating privacy, data protection, and accessibility must guide innovation, putting empowering, compassionate care in reach worldwide. Are we prepared to embrace such transformative possibilities? Beyond this point, the final revelation awaits...
The epoch of addiction recovery is witnessing seismic shifts, with innovation as its guiding force, marrying technology and holistic interventions to redefine possibilities. We've discovered that with the collective will and strategic foresight, groundbreaking care models aren't just feasible—they're rapidly materializing.
As a crucial takeaway, community-driven activism and pioneering adaptability in treatment models show profound promise for universal accessibility and impact. We all hold the key; sharing this vital knowledge can catalyze broader change. Enthusiastically spread the word, save this resource, and become a part of this transformative journey in making recovery a universally accessible reality.